Data Science as Resistance: the Urgency to Re-Design Health
Part 2: The Complexity - What We're Not Seeing, Where We Are Heading, and Action We Need Today
The Mathematics of Multi-Infection Risk: a Human Sustainability Crisis
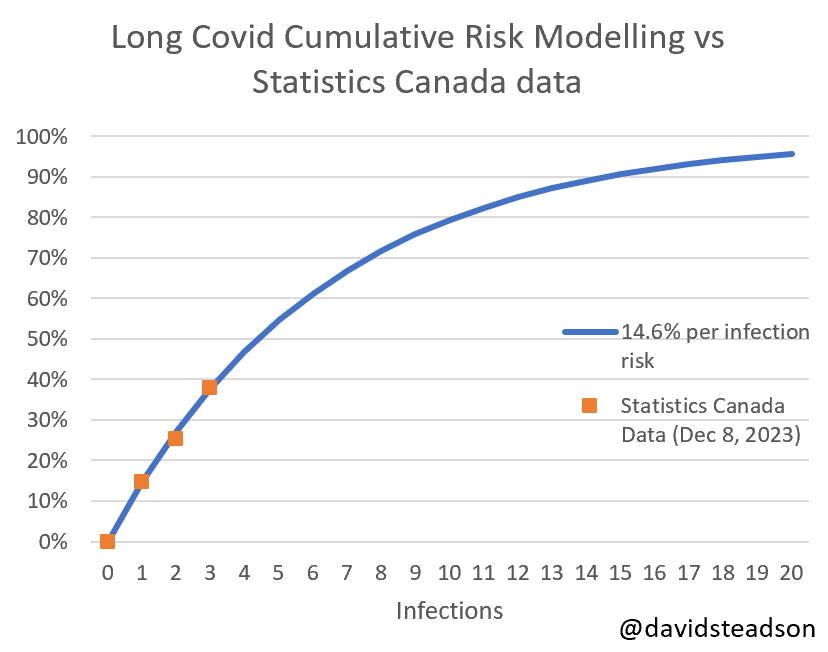
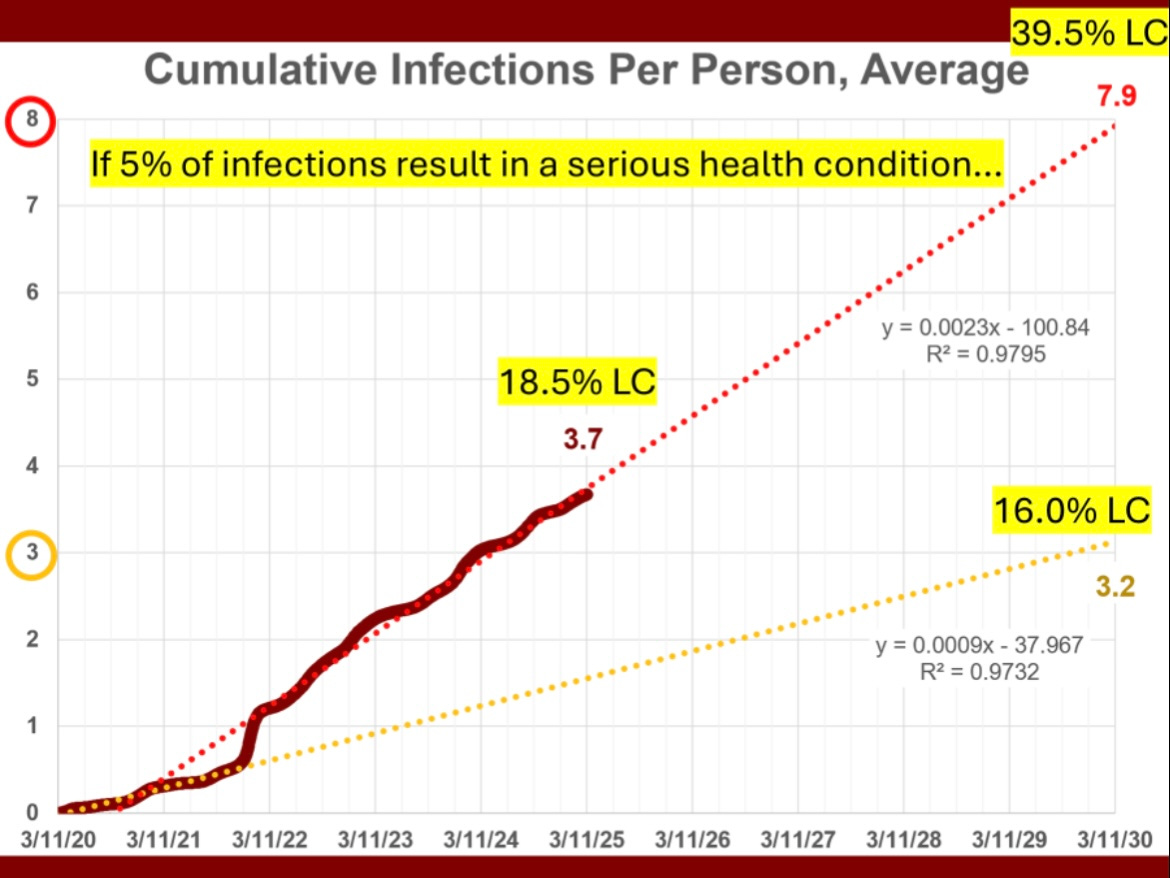
David Steadson's cumulative infection model1 reveals our approach to COVID-19 is mathematically unsustainable. By the third infection, approximately 40% of individuals develop persistent symptoms 2, with most people now averaging 3.7 infections today since the pandemic began3. This is validated by latest reports showing 1 in 3 Adults in NYC who have had a covid infection, report persistent symptoms4 and 36% globally5 are now experiencing ongoing symptoms after infection.
As presented in Part 1: Breaking the Silence on Long COVID, each reinfection accelerates biological aging, damages vital systems and our long term health6. While businesses would trigger an immediate crisis response when 40% of customers experience service failure, healthcare dismisses this data as an outlier despite affecting hundreds of millions worldwide—with an estimated cost of £20 billion per year in the UK alone7.
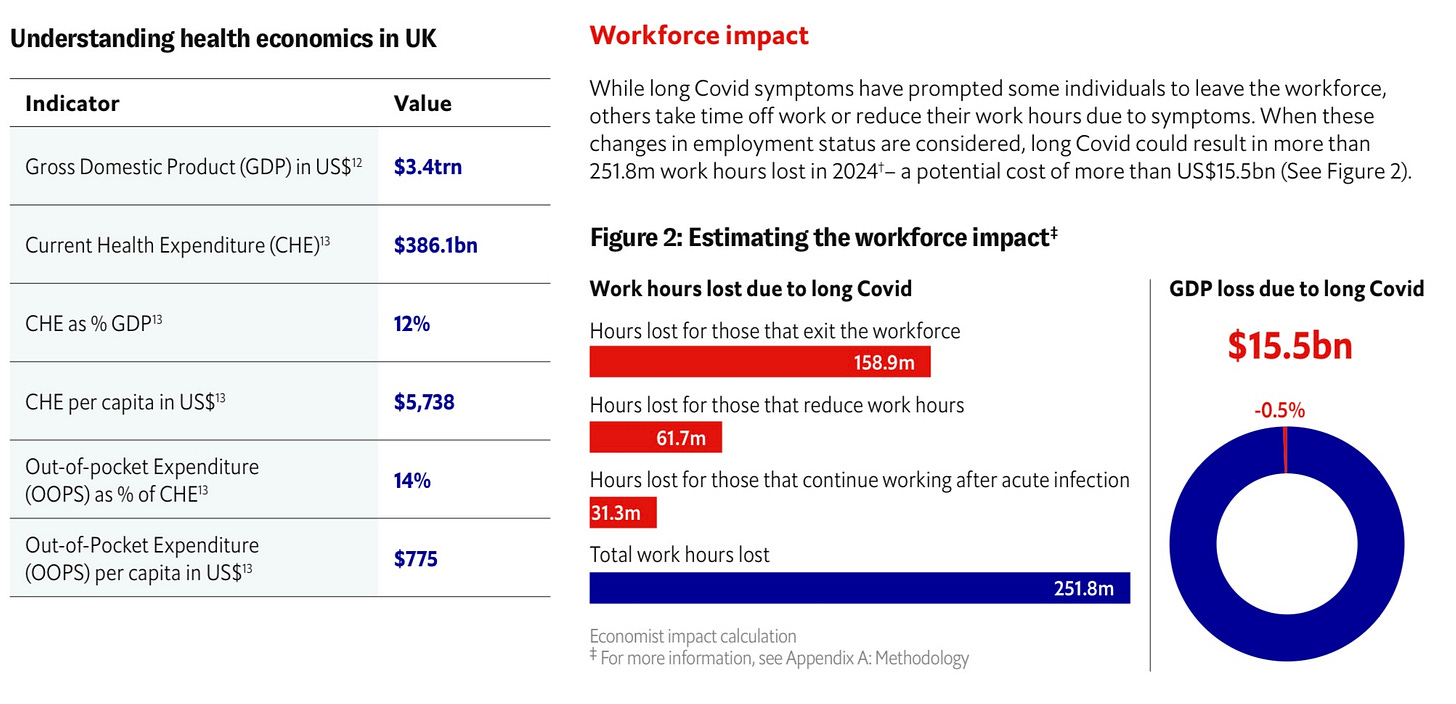
According to Economist Impact's 2024 report, Long COVID could have resulted in more than 251.8 million work hours lost in 2024 in the UK alone—a potential cost of more than US$15.5 billion in GDP loss 8 The report shows three key impacts:
158.9 million hours lost from those exiting the workforce
61.7 million hours lost from those reducing work hours
31.3 million hours lost from those continuing to work after acute infection but with reduced productivity
Additionally, Zurich UK reports claims for income protection due to long-term illness reaching record levels and SMEs picking up 73% 9of the UK sickness and absence bill in 2023.
When Enterprise Analytics Meet Personal Experience
For over two decades, I've worked at the intersection of data and human behaviour—decoding digital footprints, predicting audience behaviour, mapping emerging trends, and translating complex social dynamics into actionable insights for brands globally. This expertise in pattern and systems thinking in emerging business and innovation problems became personal when my own health collapsed in 2020, for a second time around.
Working in a bank and sustainability during the start of covid, meant that I could see spending patterns changing - and not returning, revealing what healthcare systems were missing: individuals with Long COVID and/ or the clinically vulnerable, never returned to pre-pandemic economic behaviours due to being shut out of work, health and society. Their disappearance was visible in financial data long before healthcare systems acknowledged the crisis.
This financial visibility parallels the ongoing medical invisibility. And Insurance frameworks also compound the problem— where conditions like ME and Long COVID fall through policy cracks by failing to fit into disability or recovery assumptions that are applied to all long term conditions, leaving employees without safety nets when at their most sick and vulnerable.
We are treating human health like it's unlimited, while carefully tracking, measuring and reducing environmental impacts and financial risks. By ignoring health as a further pillar of sustainability, we are creating a massive hidden health debt that doesn't show up on any corporate balance sheet - but like any debt, it will eventually come due and demand payment.
A Multi-System Challenge Requiring Multi-System Solutions
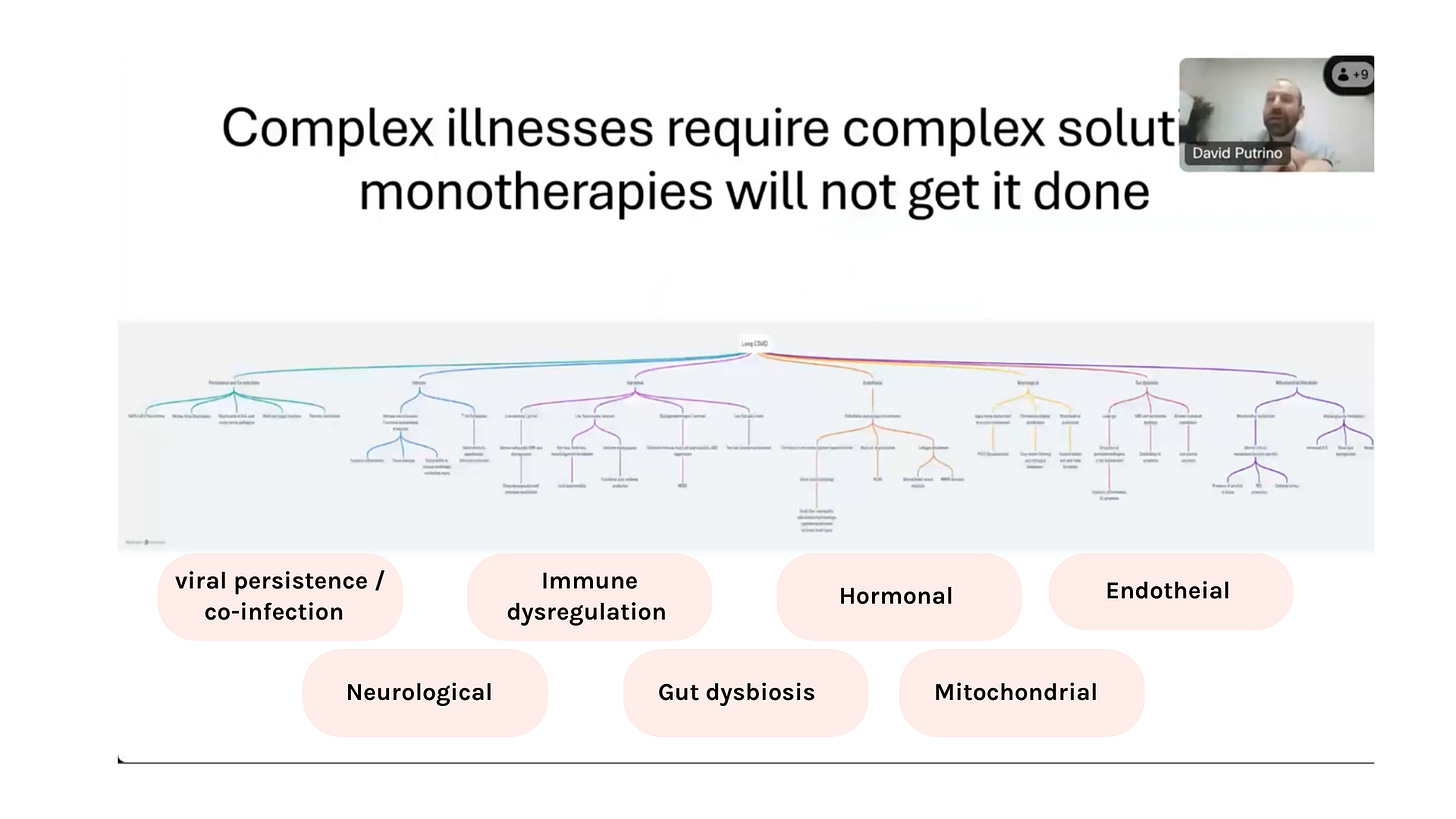
This is what is happening now with Long COVID and ME, which both involve complex interactions across multiple systems that current healthcare models are struggling to integrate and standard medical tests fail to see beyond blood:10
Viral persistence/re-infection/ co-infection
Immune dysregulation
Neurological dysfunction
Gut dysbiosis
Mitochondrial damage
Hormonal imbalances
Endothelial injury
As David Putrino, at Mount Sinai and (new) Core Sinai in NYC describes,
"Complex illnesses require complex solutions—monotherapies will not get it done." - Unite to Fight, 2024
Until we address this, policy makers and designers will continue to overlook patient complex needs, currently resulting in 98% of the clinically vulnerable feeling unsafe in healthcare settings11 and experiencing medical gaslighting12 .
(The situation is exacerbated by hospital management refusing to change their business models to protect patients and staff from repeated infections during their care, creating a dangerous cycle of exposure and deaths for the most vulnerable).13
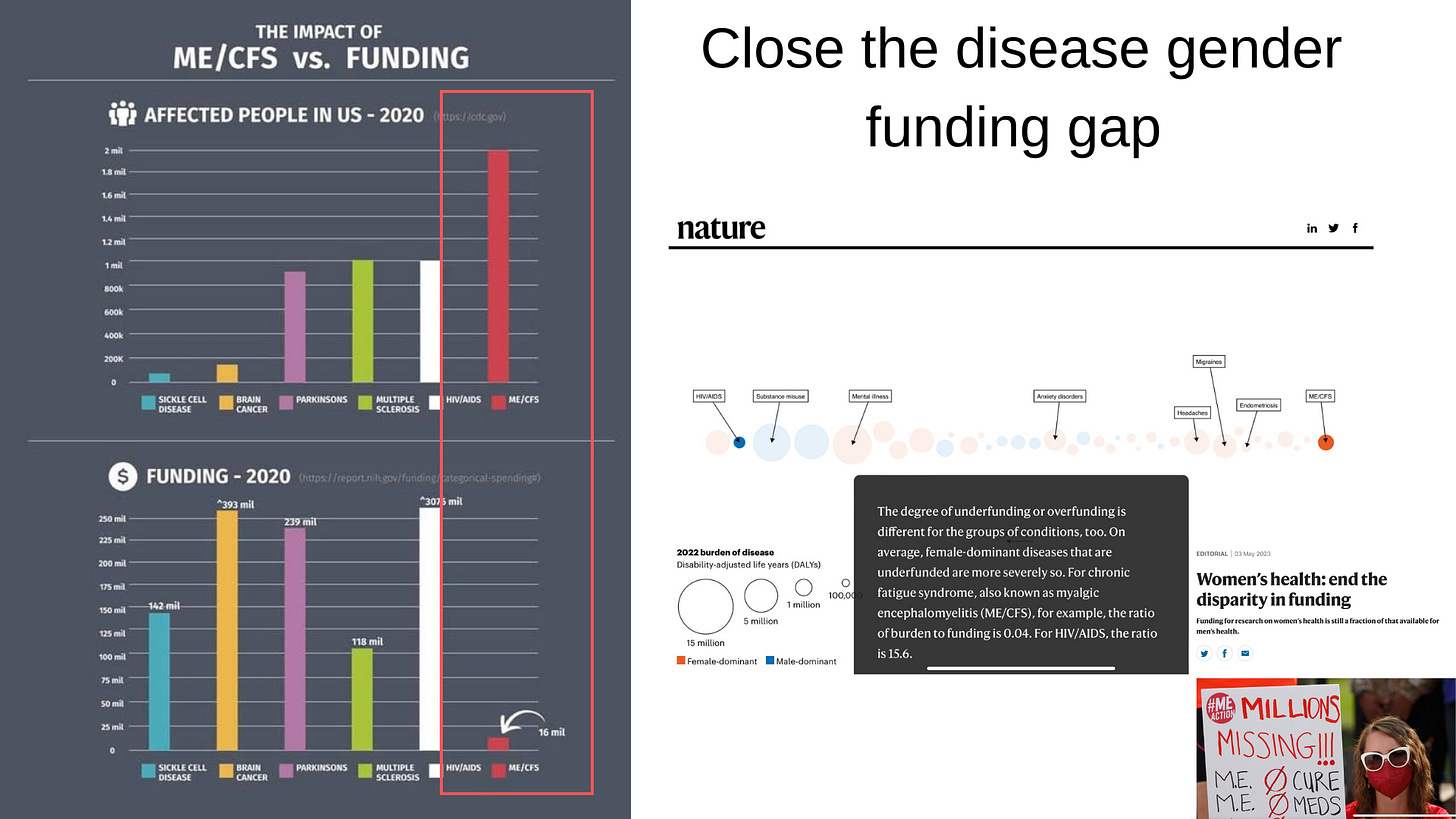
Closing the Gender Health Gap with New Field of Medicine: Infection-Associated Chronic Conditions
One of the most confronting aspects of this crisis is how it intersects with existing health inequities, particularly the $1TR gender health gap that the Mckinsey Institute of Health is working to close 14.
Pre-pandemic, ME received proportionally 390 times less funding than HIV/AIDS relative to disease burden15— particularly concerning as women have been found to be 31%16 at higher risk to develop Long Covid.
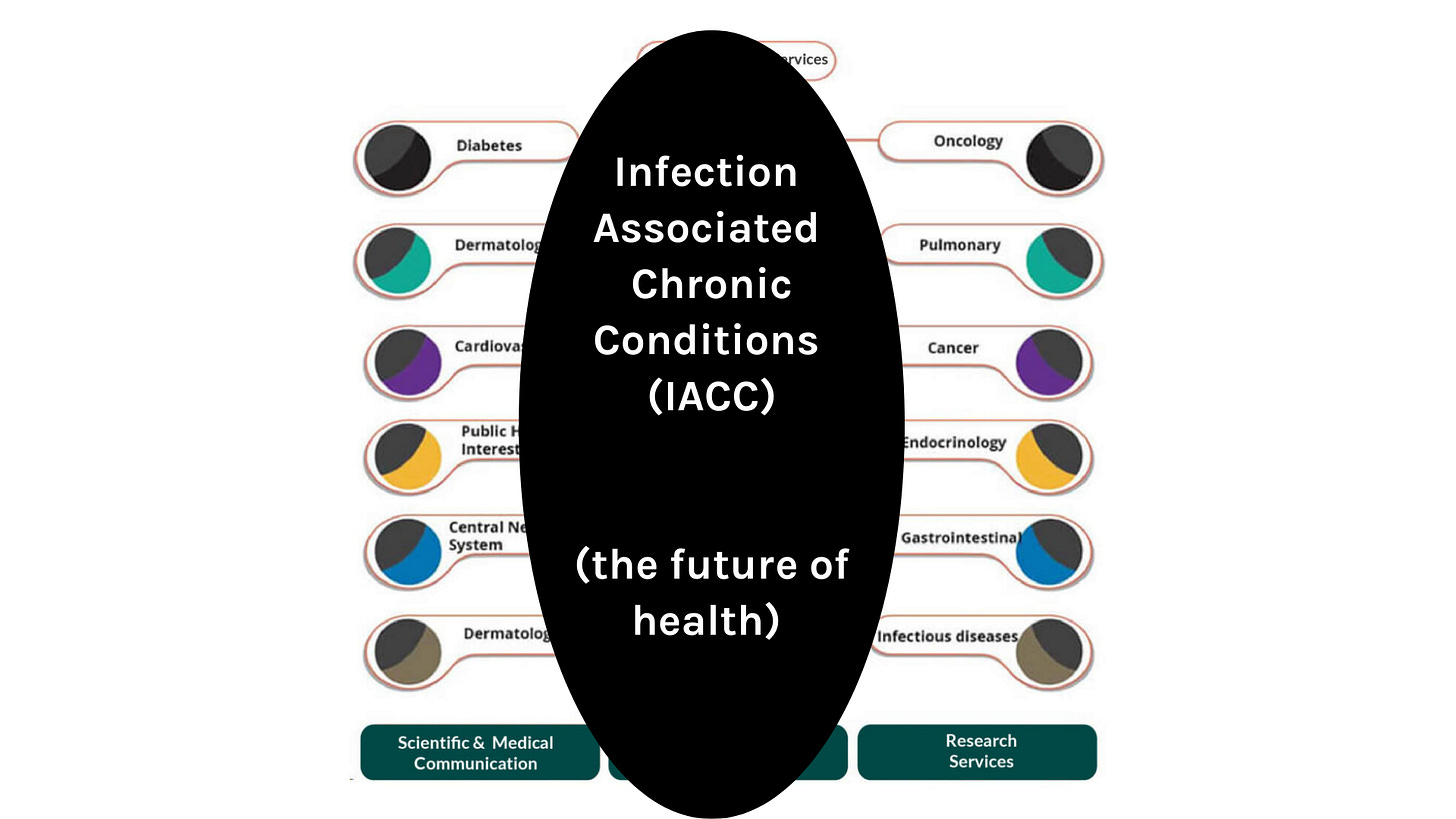
What we urgently need is a redesigned healthcare model where every specialist can recognise how infection-associated complex conditions (IACC) manifest in their field, acknowledging that SARS-CoV-2 and other viruses are directly linked to increased rates of cancers17, diabetes18, strokes19, and Alzheimer's20— triggering both new cases and accelerating disease progression.
Patient Communities as Innovation Bridges
The onset of the pandemic and my subsequent experience with Long COVID transformed my understanding of healthcare futures in deeply personal ways.
Over the last 5 years, new research and patient communities have been stepping into the void by necessity. Functioning as sophisticated research networks that collect vital data, develop innovative solutions, and challenge traditional boundaries between patients and researchers.
Patientled - led the way at the beginning of the pandemic identifying the 200+ symptoms, traditional researchers weren't aware of
PolyBio Foundation: Pioneering global collaboration examining interactions between multiple biological systems simultaneously
DeSci and Long COVID Labs: Creating decentralised science and Pharma models to accelerate clinical trials
Community Care Models (e.g Protect The Heart of The Arts): Demonstrating how built environments and the entertainment industry can adapt to safer, inclusive events and work spaces
Long COVID Moonshot and #ThereForME as patient-led political and NHS change campaigns
However, the need extends far beyond just re-designing the NHS—we must re-design health entirely.
Private healthcare systems are equally blind to infection-associated chronic conditions, whilst population health programs like Our Future Health (UK) will miss critical red flags, and even innovative insurance initiatives aimed at improving life expectancy through employee health screening are still being modelled on outdated medical text books. Meanwhile, the push for assisted dying legislation represents a profound moral failure—prioritising exit strategies over fixing broken systems that leave millions suffering without adequate care or recognition.
The Future Health Landscape: Multiple Visions Taking Shape
I am extremely fortunate to know some outstanding Futurists, Strategists, Academics and Early Adopters in my professional network, who for over a decade now have been re-imagining our future in ways most of us probably don't think about.
Through their work I am seeing multiple health future visions emerging, which only underlines the need for health to be on the business agenda and take an ecosystem approach:
The Future of Health's "live well, age well, die well" framework offers an aspirational vision for person-centred healthcare design
Wellbeing Economy movement - seeks to transform economic systems to prioritise human and planetary health over GDP growth
The longevity movement pursues breakthrough technologies to extend healthy lifespans and attracting entrepreneurs via Bryan Johnson’s ‘Don’t Die’ movement.
The exposome research community maps environmental exposures affecting health outcomes
The clean air movement is being fuelled by citizen-led design due to government inaction
UN human rights frameworks establish the right to a clean, healthy, sustainable environment
However, organisations that are investing billions in longevity and health span products and research to extend human life will be forced to watch those potential gains be systematically erased by policies that allow unlimited viral exposures.
Moving Forward: Starting with the "Unpatient"™ Population
The ongoing pandemic has created an unprecedented opportunity to redesign medicine around infection-associated chronic conditions—honouring patient expertise while embracing cutting-edge scientific approaches and systems thinking.
We should begin by focusing on the many "unpatients"—those who have fallen outside the existing healthcare system entirely (and in extreme cases, their GP's may not even know they exist)—and then work backwards to create more inclusive models.
The future of health lies in recognising that patients and doctors with lived experience, are already re-designing the systems out of necessity for themselves and others, at an incredible pace that this global emergency demands.
Healthcare and business leaders must view us as the architects and join us.
Note: Unpatient™ is new language I have created to explain the healthcare inclusion gap to business leaders and policymakers.
By Cat Fraser, (@catsocialintel)
For a deeper understanding of the healthcare impacts of this crisis, watch the second part of my presentation to the DSXHE network: Part 2 - What we’re not seeing, where we are heading and action we need today.
Resources for Part 2:
In Part 3, Learn how our innovative approaches to technology, energy-aware design and collaboration are creating a blueprint for sustainable, community-led healthcare transformation.